Knee specialist Vienna
Treatment for knee pain
Make an appointment with a specialist
Knee pain can have a variety of causes, from injuries to degenerative conditions. If you live in Vienna and suffer from knee pain, it’s important to find the right knee specialist to get an accurate diagnosis and the best possible treatment.
OVERVIEW
Are you suffering from knee pain and looking for a knee specialist?
Then you’ve come to the right place!
On this page you will find a rough overview of various knee injuries and individual clinical pictures. For more detailed information and a detailed examination of your condition, please visit me in my surgery.
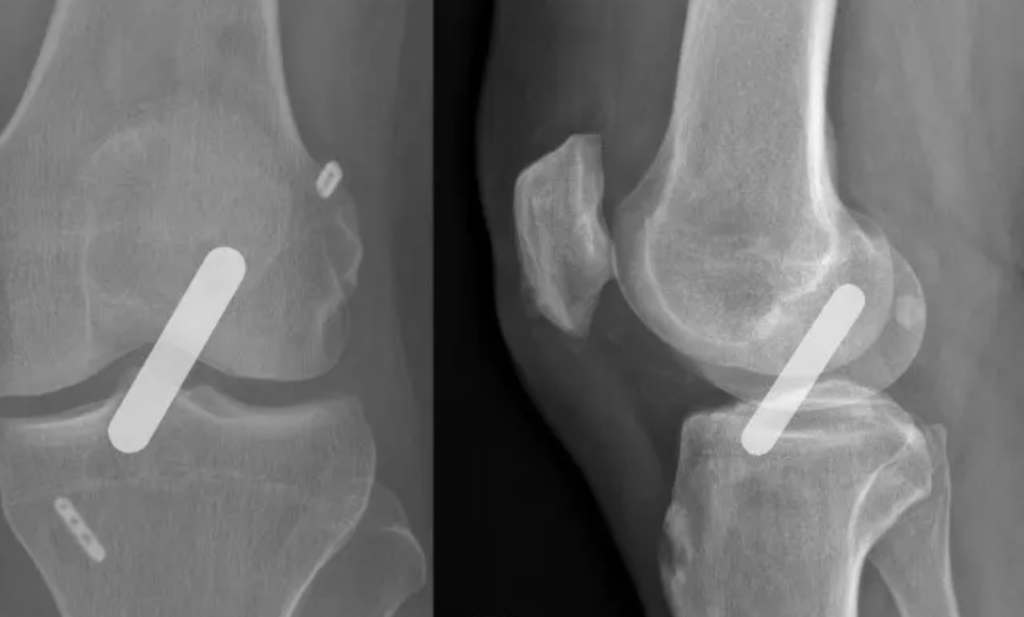
Cruciate ligament injury
Does a cruciate ligament need to be operated on?
This depends entirely on your individual requirements for your knee joint. If you are young and athletic with high sporting ambitions and are not prepared to cut back on your sporting activities, then you will clearly benefit from cruciate ligament surgery. We know from large-scale studies that very active patients with torn cruciate ligaments suffer premature destruction of the meniscus and cartilage tissue, even if no instability is subjectively noticeable.
The central and most important stabilization of the knee joint to the front and back is provided by the cruciate ligaments. A stable knee joint is therefore essential if you practice sports with many rotational movements, e.g. ball sports of any kind, especially soccer, skiing or martial arts.
I decide individually whether your cruciate ligament can be sutured (i.e. preserved) or needs to be reconstructed. It mainly depends on the type of tear, your age, your sporting ambitions and the location of the tear.
Meniscus injury
Do you have knee pain and need a professional diagnosis and targeted treatment?
A freshly torn meniscus after an accident must be examined in detail. A magnetic resonance scan shows us exactly where the meniscus is torn, how large the tear is and the shape of the meniscus tear. Based on this visualization and together with the clinical examination, we can then decide whether an operation makes sense.
Not every meniscus needs to be operated on! This is an individual decision.
If surgery is necessary, I usually try to preserve the meniscus and suture the tear . The meniscus is ultimately an important structure in the knee without which premature wear and tear of the joint cartilage occurs. Due to the specific blood supply situation, the age of the meniscus tear and your own age, it is not always advisable to suture the meniscus. Therefore, damaged parts sometimes have to be removed to prevent further damage to the joint.
“Save the meniscus” is the motto. If possible, meniscus injuries should be sutured, as the pressure ratios increase exorbitantly after meniscus resection and premature cartilage damage with resulting osteoarthritis should be avoided.
Cartilage injury
Do you have cartilage damage and don't know what to do?
It is always important to know how the cartilage damage occurred. Is it an acute injury or a sign of wear and tear? If a trauma has occurred, what was it and are there any concomitant injuries? Ligament instability (e.g. cruciate ligament rupture) or a missing meniscus are poor prerequisites for cartilage therapy. Similarly, an incorrect leg axis is not a good prerequisite for cartilage regeneration.
The leg axis, the meniscus status (in the case of cartilage damage in the knee joint) and ligament stability must be considered as part of cartilage therapy.
A distinction is made between conservative treatment with physiotherapy, nutritional supplements and infiltrations with hyaluronic acid or autologous plasma, and surgical treatment.
The following interventions are possible in cartilage therapy:
- Cartilage smoothing
- Microfracturing / nanofracturing
- Bone-cartilage transplantation
- Cartilage cultivation
- Cell-free matrix transplantation

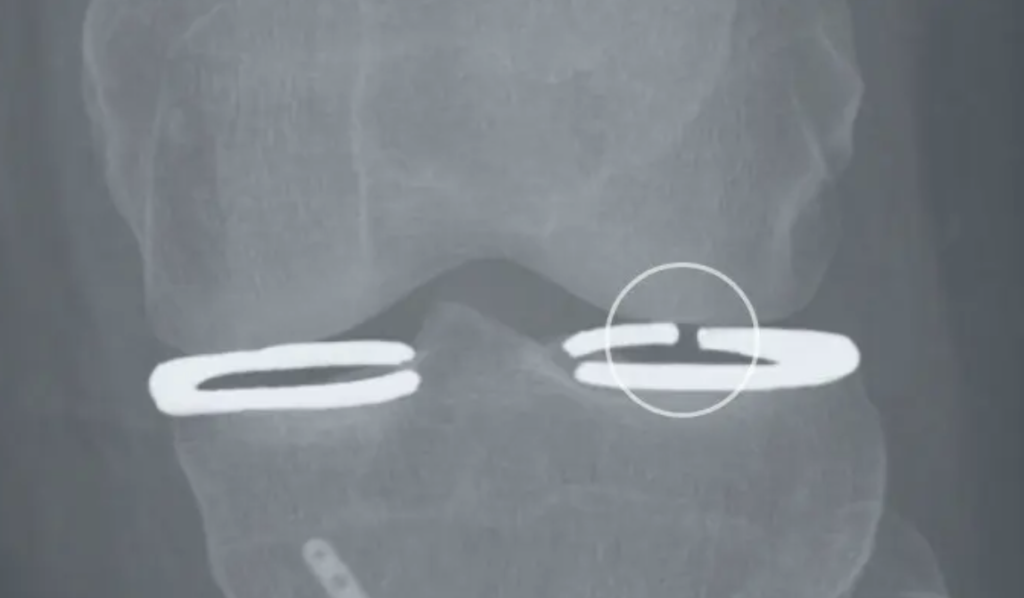
Patella instabilities
A basic distinction is made between congenital patellar instability and trauma that has caused the kneecap to dislocate outwards (patellar luxation).
Traumatic Patellar dislocations which 1st time after an adequate trauma can usually be treated mostly conservative treated. Surgical treatment is only considered in the event of permanent instability or repeated dislocations after conservative treatment.
In the case of congenital patellar instability (habitual patellar instability), the anatomy of the entire leg must be analyzed in more detail.

Autologous plasma therapy ACP
This is a new therapeutic procedure that can be used for tendon insertion irritation, muscle injuries and moderate osteoarthritis in the large joints .
Plasma is obtained by taking a blood sample, which contains an approx. 3-fold concentration of platelets. Outside the body, the platelets are activated and release a number of growth factors. These growth factors are intended to promote the proliferation of various cells (e.g. stem cells, cartilage cells, etc.), increase the formation of new blood vessels and, in particular, have an anti-inflammatory effect.
I use ACP technology in my practice because it is a closed system and no contamination from outside can occur. This is a significant advantage compared to other systems, as the safety of my patients is the most important thing for me.

Osteoarthritis of the knee joint (gonarthrosis)
Osteoarthritis is defined as a degenerative change in a joint. This leads to wear and tear of the joint cartilage until it is partially or completely depleted. As a result, the bone becomes deformed (deforming osteoarthritis) and misalignments of the leg axis worsen (bow leg, knock-kneed leg).
As with osteoarthritis of the hip joint, the joint pain is typically load-dependent, as is the initial pain in the morning, which can improve again after a little movement, depending on the extent of the osteoarthritis. The formation of effusion, which usually occurs in the evening or after excessive strain, is also characteristic of osteoarthritis of the knee. With advanced disease, many patients already complain of pain at rest , which torments them when lying down and especially at night.
It is a progressive disease with increasing symptoms. Phases of freedom from symptoms as well as intermittent exacerbations are typical.
After a precise analysis of the degree of arthrosis, your symptoms and your physical requirements, a specific therapy follows. Initially, exercise therapy ( Physiotherapy) with supportive anti-inflammatory medication. If you have already undergone this, a Infiltration cure (cortisone, hyloronic acid or autologous plasma therapy) can improve your symptoms and mobility. Only in the case of life-limiting pain, altered gait pattern or reduced walking distance does the artificial knee joint replacement (endoprosthesis, K-TEP) as a last resort.

The runner's knee
Runner’s knee, also known as patellofemoral pain syndrome, is a common complaint among runners. It occurs when the kneecap does not slide optimally in the femoral groove and causes friction. A typical symptom is anterior knee pain, especially when climbing stairs, kneeling or sitting for long periods. The causes can be varied, including muscle weakness, misalignment or overuse due to intensive walking activities. A precise diagnosis is crucial in order to select suitable treatment approaches. Physical therapy to strengthen the muscles, targeted training and adjustments to walking technique are often part of the treatment plan. With the right care, many sufferers can continue their running activities without pain and minimize long-term discomfort.

No matter what type of knee pain you suffer from, seeing a knee specialist in good time is crucial to avoid intense pain and counteract long-term knee problems.
The knee is a very complex joint – so choose your doctor wisely! I have assisted countless patients in the treatment of knee pain and given them the help and support they needed to recover from a knee injury.
As a knee surgeon and head of the MSV surgery, I offer complete care for your knee injury – from the initial anamnesis to physiological care after the operation – all under one roof.
FAQ - Knees & knee pain
How does the knee work and how is it structured?
The knee joint is a complex joint that enables movement and provides stability at the same time. It is made up of various components: the thigh bone (femur) as the upper part of the joint, the tibia (shin bone) as the lower part, and the kneecap (patella) in front of the joint. The menisci, crescent-shaped cartilage discs, are located between the femur and tibia and are used for stabilization, cushioning and load distribution.
In addition, various ligaments provide stability. The collateral ligaments (medial and lateral collateral ligaments) prevent lateral movements, while the anterior and posterior cruciate ligaments (anterior and posterior cruciate ligaments) control rotation and forward and backward movements. The joint capsule surrounds the knee joint and contains synovial fluid for lubrication.
The functioning of the knee joint involves flexion and extension, enabling basic activities such as walking, running and jumping. It also allows limited rotation and turning movements, with the menisci distributing loads evenly. The stability of the joint is provided by muscles, ligaments and balanced musculature. Problems such as injury or arthritis can lead to knee pain and impairment, so it is important to seek medical advice in such cases.

What are the most common causes of knee pain?
The most common causes of knee pain can be many and varied. Here are some of the most common reasons:
-
Injuries: Traumatic injuries such as sprains, strains, torn meniscus or torn ligaments can lead to acute knee pain.
-
Arthritis: Osteoarthritis (wear and tear of the cartilage) and rheumatoid arthritis (inflammatory joint disease) can lead to chronic knee pain.
-
Overloading: Excessive strain due to intensive training, especially in running sports (runner’s knee), can lead to overuse syndromes such as patellofemoral pain syndrome.
-
Age: With increasing age, the risk of degenerative changes in the knee increases, which can cause pain.
-
Poor posture and misalignment: Unfavorable postures and anatomical misalignments, such as knock knees or bow legs, can contribute to knee pain.
-
Bursitis: Inflammation of the bursa in the knee can cause pain and swelling.
-
Cartilage damage: Injuries or wear and tear to the cartilage in the knee can lead to pain and limited mobility.
-
Infections: Infections in the knee joint can lead to inflammation and pain, but usually require immediate medical attention.
-
Kneecap problems: Problems with the position or movement of the kneecap can lead to pain, especially when bending or extending the knee.
-
Tumors: Although rare, malignant tumors in the knee area can cause pain.
How can I distinguish between acute knee pain and chronic complaints?
Distinguishing between acute knee pain and chronic pain is important in order to initiate appropriate treatment. Acute knee pain occurs suddenly, often in response to an injury or a specific strain. This pain is usually short-lived and can be improved with rest, ice, compression and elevation measures (PECH rule). There is often a clear trigger, such as a fall, blow or sudden movement, and people with acute knee pain may have no or only a short history of knee problems.
In contrast, chronic knee pain develops gradually over a longer period of time and can be recurrent. This type of pain lasts for an extended period of time and may not fully improve with rest and simple home remedies. Chronic knee pain can occur during everyday activities such as walking, climbing stairs or sitting, even without an obvious trigger. People with chronic knee pain often have a history of knee injury, arthritis or other long-term knee problems. It is important to note that this distinction is not always clear, and it is recommended to see a doctor to get an accurate diagnosis. A specialist will be able to make an informed assessment through clinical examination, imaging and medical history and recommend an appropriate treatment strategy.
What role do muscle weaknesses play in knee problems?
Muscle weaknesses play a crucial role in knee problems. The muscles around the knee joint play an important role in stabilizing and supporting joint function.
How can I protect my knee from injury during training or sport?
Protecting the knee during exercise or sport is crucial to avoid injury. Here are some tips to protect the knee structure:
-
Warm up: Start your training or sports activities with an appropriate warm-up program. Dynamic stretching and light cardio exercises increase blood circulation and prepare the muscles and joints, including the knee, for exertion.
-
Strengthening exercises: Strengthen the muscles around the knee joint, especially the quadriceps and thigh muscles. Targeted exercises such as squats and lunges help to improve knee stability.
-
Correct technique: Make sure that you use the correct technique for all exercises and sporting activities. Incorrect execution can put excessive strain on the knee and lead to injury.
-
Suitable footwear: Wear well-fitting and supportive footwear that stabilizes the foot and knee. The right shoes can help to minimize the strain on the knee.
-
Progressive load: Increase the intensity and duration of your training sessions gradually. Avoid abrupt, drastic changes to prevent overloading and injuries.
-
Breaks and relaxation: Plan sufficient breaks and recovery phases between training sessions. This gives the muscles and joints, including the knee, the time they need to regenerate.
-
Proper footwear: Make sure that your shoes meet the requirements of your sport. Special sports often require specific footwear that better protects the foot and knee.
-
Cooling after training: After exercise, applying cold packs to the knee can help reduce swelling and promote recovery.
-
Controlled movements: Carry out all movements in a controlled and careful manner. Avoid jerky or excessively fast movements that could strain the knee.
-
Professional guidance: If you are unsure about the correct technique or exercise program, seek advice from a qualified trainer or a subject matter expert who can give you specific guidance.
By incorporating these tips into your exercise routine, you can minimize the risk of knee injuries and promote the health of your knee during exercise or sports.
How do I get back to my old form after a knee injury?
Recovery after a knee injury requires patience, time and a structured rehabilitation strategy. Physiotherapy can help to rebuild the muscles in the thigh and improve stability in the knee. At my practice in 1030 Vienna, I work with great physiotherapists who will help you to relieve the pain in your knee and get back to your old shape.