Osteoarthritis of the hip (coxarthrosis)
Conservative treatment & prosthesis fitting
ÜBERSICHT
Osteoarthritis of the hip joint - coxarthrosis
Osteoarthritis is defined as a degenerative change in a joint. This leads to wear and tear of the joint cartilage until it is partially or completely depleted. As a result, the bone becomes deformed (deforming osteoarthritis) and pitted (debris cysts).
Hip osteoarthritis develops gradually and usually over a period of years. In the early stages, osteoarthritis causes hardly any discomfort. However, as the cartilage wears away, patients feel pain and are restricted in their mobility. In many cases, physiotherapy and a change in diet and lifestyle can help to slow down or stop the progression of hip osteoarthritis. If the disease has progressed to an advanced stage, hip treatment specialists can use surgical procedures such as hip arthroscopy, cartilage transplantation or hip prostheses to restore mobility. This helps patients achieve pain-free movement and an improved quality of life.
I – Dr. Gustav Timmel – am an expert in the treatment of osteoarthritis of the hip joint and would like to help you lead a pain-free life! Contact me and I will ensure you receive individual treatment tailored to your needs!
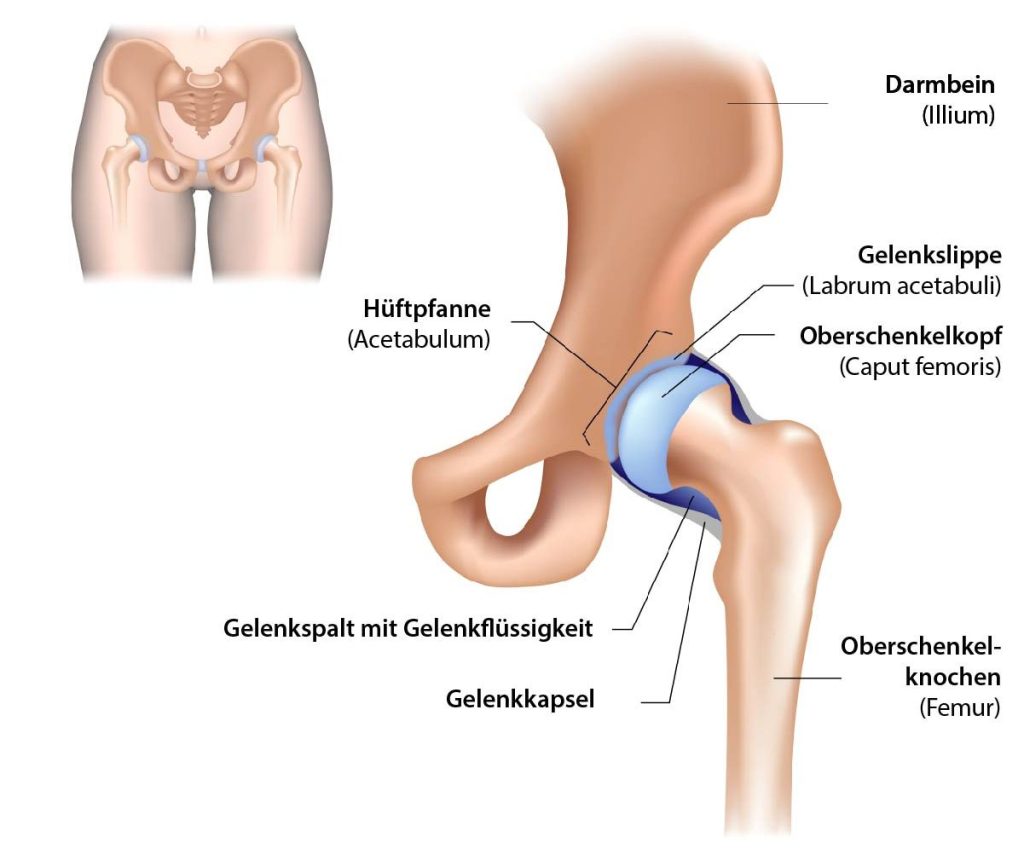
Anatomy of the hip
The hip is a ball-and-socket joint located between the thigh bone (femur) and the pelvis. The socket, called the acetabulum, holds the ball of the femoral head in position and provides stability when moving the legs. Both parts of the joint are surrounded by a layer of cartilage that protects them from wear and tear and enables smooth and pain-free movement.
What is hip osteoarthritis (coxarthrosis)?
Hip osteoarthritis or coxarthrosis is a type of osteoarthritis that affects the hip joint. It occurs when the cartilage between the bones in the hip joint wears away over time (joint wear and tear). This is why it is also described as a degenerative disease of the hip joint.
This causes pain and stiffness as the bones rub against each other, leading to swelling and inflammation. The most common risk factor for developing hip osteoarthritis is age, as it usually occurs from middle age onwards. Other contributing factors include obesity, genetic predisposition, gender, previous injury or trauma to the area or certain conditions such as rheumatoid arthritis or diabetes.
Symptoms of hip osteoarthritis (coxarthrosis)
The remodeling processes of the bones cause the ball and socket joint to deform, resulting in load-dependent joint pain, joint stiffness and restricted range of motion. Characteristic symptoms are morning start-up pain, which can improve again after a little movement, depending on the extent of the osteoarthritis.
The pain is often perceived as “dull” and “deep-seated”. It is projected onto the groin area and often into the knee joint. It is not uncommon for patients to present with knee pain whose cause is actually in the hip joint. With advanced disease, many patients already complain of pain at rest , which torments them when lying down and especially at night. It is a progressive disease with increasing symptoms. Phases of freedom from symptoms as well as intermittent exacerbations are typical.
Symptoms at a glance
- Start-up pain
- Load-dependent joint pain
- Joint stiffness
- Restriction of the range of motion
- Groin pain
- Problems putting on shoes or socks
- Pain when descending (e.g. stairs)
- intermittent exacerbations
Who is affected by hip osteoarthritis (coxarthrosis)?
Studies show that 3-6% of the population suffer from osteoarthritis of the hip joint. In most patients, it occurs after the age of 50. To a certain extent, everyone’s ability to use the hip joint decreases with age. This is initially normal and treatment is not necessary. The orthopaedic surgeon is only a good point of contact for treatment options when performance and load-bearing capacity are significantly below age-appropriate expectations.
The risk of coxarthrosis increases with age – the older a patient is, the more likely it is that they will develop hip osteoarthritis requiring treatment. In general, it can be said that in most cases there is a specific cause for the disease. Statistically speaking, people who put a lot of strain on their hips due to their job or sport are more likely to have problems with osteoarthritis of the hip joint. People of European descent are more likely to develop primary osteoarthritis than people from Asia or Africa. And if your hip is already damaged – due to an accident or a disease such as dysplasia – you are also more likely to develop osteoarthritis of the hip.
Causes & risk factors at a glance
- Advanced age (from 55 years)
- Gender (women are more frequently affected)
- Overweight (obesity)
- Heavy strain due to work or sport

Coxarthrosis - progression and stages
The stages of hip osteoarthritis depend on how far the wear and tear of the hip joint has already progressed. Articular cartilage is a type of connective tissue which, the older a person gets, the less water this tissue can form – it gradually becomes less and less elastic.
This process can be compared with an example from dermatology! The older we get, the more wrinkles we get. This is because wrinkles also occur as a result of the increasingly less elastic connective tissue under the skin. Hip osteoarthritis is therefore a symptom of old age, just like wrinkles. Nevertheless, there are individual factors that promote osteoarthritis of the hip, such as lack of exercise, obesity, incorrect loading and/or overloading.

Stage 0 - Healthy hip joint
The hip shows no signs of coxarthrosis. The cartilage is smooth and elastic.
Stage 1 - No pain
The cartilage surface appears to have rough patches and the surrounding tissue looks damaged. At this stage, osteoarthritis of the hip joint is usually only discovered by chance, as the affected person does not experience any pain.
Stage 2 - Restrictions and start-up pain
The first pain already occurs at this stage. This is where the so-called start-up pain or movement restrictions caused by hip osteoarthritis become noticeable.
Stage 3 - inflammation, pain even at rest
As soon as this stage is reached, around 50-100% of the cartilage layer is damaged, as the connective tissue is dissolved and the cartilage is broken down. Pain is now also noticeable at night – osteoarthritis of the hip shows significant limitations for the person affected.
Stage 4 - "cartilage baldness"
The cartilage layer has been removed to such an extent that the bone is exposed and bone rubs directly against bone.
Diagnosis of hip osteoarthritis
During the clinical examination , characteristic pain can be triggered, particularly during internal rotation of the hip joint. At an advanced stage, comparatively severe movement restrictions may be noticeable, which are also perceived as disturbing in everyday life. Specific x-rays are usually sufficient to confirm the clinical diagnosis.
The first radiological signs of hip osteoarthritis are joint space narrowing and subchondral sclerosis. Debris cysts, osteophyte formation and a rounded femoral head are seen at an advanced stage.


Treatment of osteoarthritis of the hip joint
In the early stages , conservative therapy is always in the foreground. The initial symptoms can be alleviated and the intermittent progression controlled with physiotherapy exercises and temporary intake of anti-inflammatory medication. If this no longer leads to the desired success, injections of cortisone directly into the joint (intra-articular) can be administered to support the anti-inflammatory effect. Injections with hyaluronic acid and autologous plasma (ACP) are also a good way of alleviating pain and offer a good option for conservative treatment of hip osteoarthritis (coxarthrosis).
With increasing suffering and life-limiting pain , the last option is an artificial joint replacement(hip prosthesis). The X-ray image only gives an indication of the extent of the osteoarthritis. The pain and changes to everyday life are problematic for each patient individually, so the indication for surgery is determined together with the patient. The timing of the operation YOU decide
Hip joint replacement / total hip joint endoprosthesis H-TEP
The artificial replacement of a joint is a standardized procedure. Patients with hip pain in particular are satisfied in over 90% of cases due to the minimally invasive surgical approaches, which spare the muscle groups around the hip. Hip prostheses are planned by me in advance using a standardized planning X-ray and the prosthesis size and position are determined individually. Only then can the best possible result be achieved. A muscle-sparing surgical approach (minimally invasive) is now standard.
In classic hip surgery, the damaged femoral head and part of the neck of the hip joint are removed and then the acetabulum is drilled out. Finally, two components of an artificial hip joint (prosthetic head and socket) are anchored in the bone to relieve you of your pain.
After the operation, most patients are usually independently mobile again within a few days with 2 forearm crutches. These should be used for 6 weeks to reduce the load on the new joint. This helps the prosthesis to grow into the bone correctly and enables the hip prosthesis to last a long time.
Within the first 3 months, further rehabilitation as part of inpatient rehabilitation has proven successful.
Frequently asked questions:
The minimally invasive surgical approach does not necessarily describe the size of the scar or the skin incision, but rather the muscle-sparing surgical approach. No muscle is cut, but an access between individual muscle groups is used to reach the hip joint.
A regularly fitted hip prosthesis has a lifespan of approx. 15-20 years. In some cases even longer. Of course, this also depends on the individual load on the hip joint. If sports that put a lot of strain on the joint are practiced regularly, the wear and tear on the mechanical components is greater than with a quieter lifestyle.
The hip prosthesis is made up of 4 main components: The stem and the acetabulum are made of a bone-friendly titanium alloy. The surface is specially coated to accelerate and reinforce ingrowth into the bone. The inlay anchored in the cup and the femoral head attached to the stem are the actual joint partners (sliding pair) of the hip prosthesis. Nowadays, ceramic-ceramic orpolyethylene-metal pairings are mostly used, as both pairings are extremely wear-resistant.
In principle, most sports are possible again after a successfully implanted prosthesis. Excessive strain should be avoided in the first 6 months after the operation.
Sports with little strain on the hip joint:
- Cycling
- Nordic Walking
- Hiking
- Swimming
- Rowing
- Golfing
Sports with more load (=lower service life of the prosthesis):
- Alpine skiing
- Martial arts
- Tennis
- Other sports with “stop and go” movements
Partial weight-bearing with 2 forearm support crutches should be maintained for 4-6 weeks after the operation. The prosthesis needs this time to bond firmly with the bone.
Frequent symptoms
Lateral hip pain
(trochanteric bursitis, tendon insertion irritation): There is often a muscular imbalance with insufficiency of the gluteus medius. This can be detected with a clinical examination, so that not only infiltrations but also special muscle training can be the key to success.
Sports bar
This describes a tissue weakness of the fascia in the groin area without the usual hernia sac. As there are no muscular parts of the abdominal wall here, this area cannot be strengthened with muscle training. The cause may be trauma or a general weakness of the tissue.
