Cruciate ligament rupture Vienna
Treatment & cruciate ligament surgery
Acute care & follow-up treatment
Anterior cruciate ligament rupture (= cruciate ligament rupture) is one of the most common sports injuries. Around 80% of the normal population can return to sport after a cruciate ligament injury, but only around 55% of athletes return to their previous sporting level. Constant ligament instability, particularly during sporting activity, leads to premature wear of the cartilage and meniscus and thus to joint degeneration over time. joint wear and tear . Cruciate ligament surgery is usually the only way for many athletes to be able to fully pursue their passion again. Find out more below!
OVERVIEW
Does a torn cruciate ligament require surgery?
Are you young and athletic, have high sporting ambitions and are not prepared to cut back on your sporting activities? Then you will clearly benefit from cruciate ligament surgery. We know from large-scale studies that very active patients with torn cruciate ligaments can suffer premature destruction of the meniscus and cartilage tissue, even if no instability is subjectively felt. So if you play sports with a lot of rotational movements, e.g. ball sports of any kind, especially soccer, skiing or martial arts, a stable knee joint is essential.
I decide individually whether your cruciate ligament can be sutured (refixed) or reconstructed (tendon replacement surgery). The type of cruciate ligament surgery depends mainly on the type of tear, your age, your sporting ambitions and the location of the tear.
If you have a sedentary job and no ambition to be active in sport or are prepared to reduce your sporting activities, you do not necessarily need to have surgery on your cruciate ligament. Targeted muscle building and physiotherapy training can achieve very good results even without surgery. However, if you notice so-called “giving way attacks” (buckling of the knee joint), surgery should be discussed again, as this is a sign of rotational instability of the knee joint.
This so-called instability is a rotational movement between the thigh and lower leg that leads to premature wear of the joint cartilage and meniscus.
Your specialist for cruciate ligament ruptures
Find out more about cruciate ligament surgery & treatment for a torn cruciate ligament in this video!
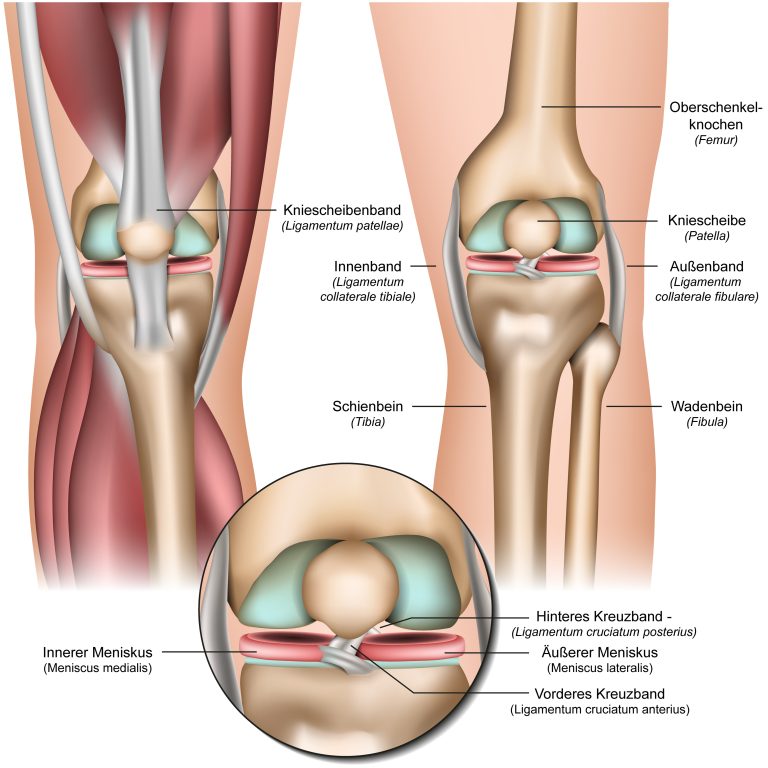
What is a cruciate ligament?
The cruciate ligament is a complex interplay of bones, ligament complexes, muscle attachments and tendons. The knee joint can thus be stabilized even under maximum load, e.g. during sport. A simplified distinction is made between 4 main ligaments which protect the knee against rotation and axial tilt.
The most important ligaments in the knee are the anterior and posterior cruciate ligaments, which cross inside the joint and are responsible for stabilizing and controlling forward and backward movements.
The anterior cruciate ligament runs diagonally through the knee joint, originates from the inside of the lateral (= outer) femoral condyle and attaches centrally to the tibial plateau (eminentia intercondylaris). It consists of 2 main bundles: the anterolateral and the postermedial bundle. Depending on the degree of flexion of the knee joint, the bundles are tensioned to different degrees.
The anterolateral bundle is mainly responsible for the anterior translation (= advancement of the tibial plateau in relation to the femur) of the tibial plateau. The significantly shorter postermedial bundle is thought to inhibit internal rotation.
The cruciate ligament lies in the middle of the knee joint and is surrounded by synovial fluid (= joint fluid). For this reason, no blood clot can form, which would be so important for healing.Spontaneous healing of the ligament is therefore almost impossible.
Cause of a torn cruciate ligament in the knee
Athletes between the ages of 15 and 25 are most frequently affected, as the demand on the knee joint is particularly high at this age due to sporting ambitions. Female athletes are up to 5 times more likely to suffer a cruciate ligament injury than males. This is attributed to a weaker connective tissue, but also to a more frequent occurrence of an X-leg.
A torn cruciate ligament often occurs in sports with many changes of direction, i.e. typical stop and go sports with sudden turning movements, such as soccer, handball or basketball. The body’s centre of gravity is usually further back, the knee joint is slightly bent, the foot is fixed to the ground and the knee is forced valgus (=X-leg) and outwards.

- Landing on one leg after a jump
- Sudden stop
- Sudden rotational movements
In skiing, the knee is usually bent more, the center of gravity is further back, while the knee is rotated inwards. This is known as the phantom foot mechanism or dynamic snowplow. However, classic “threading” through a valgus (=X-leg) and external rotation can also lead to a rupture of the anterior cruciate ligament.
Accident mechanisms Ball sports
Landing on one leg after a jump
Sudden stop
Sudden turning movements
Skiing accident mechanisms
Classic "threading"
Dynamic snow plow
Hyperextension of the knee joint
Diagnosis of a cruciate ligament rupture
A suspected cruciate ligament rupture can already be diagnosed based on the medical history and the mechanism of the accident. Clinical examination by a specialist remains essential. Various clinical tests(Lachman test, pivot shift test, anterior drawer) can be used to evaluate the stability of the cruciate ligament and the entire knee joint.
One of the most informative tests is the Lachman test, which involves subjectively measuring the propulsion of the lower leg against the thigh. In comparison to the opposite side, the increase in the forward thrust is indicated in + (5mm), ++ (10mm) or +++ (>10mm). In addition, the quality of passive tensing can be specified as “firm stop”, “soft stop” or no stop.
The pivot shift test allows the examiner to objectively assess rotational instability. This test can also be given in 3 grades, but is often not feasible in the acute injury situation due to the pain. A positive test reflects the extent of the rotational instability and usually results in reconstruction of the cruciate ligament.
Radiologically, a magnetic resonance imaging (MRI ) scan is required to confirm the clinical diagnosis and to visualize the tear and any accompanying injury.
Cruciate ligament rupture patients can be divided into 3 groups can be distinguished:
- The COPER: Conservative therapy alone can restore previous sporting activity.
- The NON COPER: Complain of knee joint instability and cannot return to their usual sport. Sometimes the feeling of instability (giving way attacks) is a problem even in everyday life. Surgery should be recommended for this group to prevent chronic wear and tear of the cartilage and meniscus.
- The ADAPTORs: Adapt their sporting activities so that no instability occurs. This group can also be treated primarily conservatively.

Unfortunately, no test can currently differentiate between COPER and NON COPER. If giving way attacks occur during the course of conservative treatment, a change of therapy from conservative to surgical treatment should take place.
It is now known that the probability of cartilage or meniscus damage over the course of 10 years is up to 6 times higher after conservative treatment of a cruciate ligament injury compared to the surgical group. Therefore, young athletes with many stop at GO movements who wish to continue practicing the sport should be recommended cruciate ligament reconstruction.
Concomitant injuries should also be included in the choice of therapy, as additional meniscus damage or collateral ligament injuries can also destabilize the knee joint.
“Not every cruciate ligament rupture requires surgery, but an unstable joint should be stabilized!”
How do I recognize a cruciate ligament rupture?
Many athletes feel a snap in the event of an accident, which is accompanied by an immediate effusion of the knee joint. A hemarthrosis (= bloodyeffusion of the joint) indicates a torn anterior cruciate ligament until proven otherwise. The loss of the stabilizing function of the ligament can result in “giving way attacks”. These are rotational movements between the thigh and lower leg which, if left untreated, lead to the destruction of the meniscus and cartilage tissue.
Symptoms of a cruciate ligament rupture
Various symptoms can occur with a cruciate ligament rupture, including sudden and severe pain in the knee, swelling, instability of the joint, a feeling of joint dislocation or “popping”, limited mobility and a cracking sound during the injury. Bruising may also occur in the knee area. It is important that a torn ACL is diagnosed and treated by a medical professional, as appropriate rehabilitation and possibly surgery may be required to restore stability and function to the knee joint.
Treatment of a cruciate ligament rupture
Depending on the patient’s age, sporting ambitions, profession and additional concomitant injuries, the decision on therapy is discussed individually with the patient.
There are 3 therapeutic options:
- Conservative therapy
- Surgical cruciate ligament refixation (cruciate ligament suture)
- Surgical cruciate ligament replacement
Conservative treatment of cruciate ligament rupture

Just because no surgery is performed does not mean that no therapy is necessary. Quite the opposite! Immediately after the injury, the swelling and pain should be treated with cooling and compression. Physiotherapy must then be started as soon as possible to restore the normal range of movement. The knee flexor muscles on the back of the thigh should be strengthened in comparison to the quatriceps. As they pull the lower leg backwards, they have a cruciate ligament-protective effect. Proprioceptive training improves depth perception with the help of balance and concentration exercises and should also be incorporated into conservative therapy.
The stability of the joint should be continuously checked during the course of the treatment in order to evaluate the indication for conservative therapy.
Can a torn cruciate ligament also be stitched?
Not every cruciate ligament can be reattached! This depends on the age of the patient, the time of the injury and the location of the tear. Only cruciate ligaments that are torn directly from the bone show good long-term results. Tears in the middle of the ligament should rather be treated with a replacement.
The timing is crucial! Only injuries that are reattached to the bone in the first 3 weeks are likely to be successful. It is also known that the probability of a cruciate ligament suture failing again is higher than that of a cruciate ligament plastic tearing again. It is therefore better to refrain from cruciate ligament sutures in young athletes.
WHEN IS A SUTURE POSSIBLE?
Patient age (>25)
Surgery Within 3 weeks
Torn off directly at the bone
What is cruciate ligament replacement surgery?
In an arthoroscopic cruciate ligament reconstruction, a tendon from the patient’s own body is removed and then inserted as a new cruciate ligament in place of the tornone (cruciate ligament replacement surgery)
The sports orthopaedic surgeon has several options when choosing a graft. The hamstring tendons (semitendinosus and gracilis tendons STG), part of the quatriceps tendon or the middle third of the patellar tendon BTB are available. In revision cases (= second operation) or if all other tendons are to be spared, an allogenic force (= donor tendon, a specifically processed cadaveric tendon) can also be used. They all have different advantages and disadvantages, which is why the choice of tendon should be an individual decision.

Which tendon for cruciate ligament replacement surgery?
Hamstring tendons (semitendinosus and gracilis tendons STG): This is the standard tendon used by many sports orthopaedic surgeons to reconstruct a torn cruciate ligament. The tendon is harvested through a 2-3 cm incision on the inside of the tibial plateau or just above the popliteal fossa (post-medial harvesting), folded several times and reinforced with a special suture construct. If the graft is too small, the gracilis tendon can also be harvested through the same incision to reinforce the graft.
Tendon removal results in a maximum loss of strength of 10% when flexing the knee, which is usually not noticed by amateur athletes. Particularly in the case of a pre-existing knock-knee or additional injury to the medial collateral ligament, the inner side should not be further weakened by tendon removal. Even if there is no scientific evidence in this regard, I use a different graft in these cases.
Patellar tendon (=patellar tendon) BTB ( =bone tendon bone): In a patellar tendon graft, the middle third of the tendon is harvested with a bone block from the kneecap and another bone block from the tibial plateau.
One advantage is the faster return to sport compared to other grafts, as the bone blocks grow into the bone canals faster than other cruciate ligament grafts.
A disadvantage is the anterior knee pain that often remains, which causes pain especially when kneeling. A loss of strength of approx. 10% when extending the knee can also remain, which can cause problems, especially in jump-dominant sports.
Quadriceps tendon: The middle superficial third of the quadriceps tendon is harvested through an approx. 3-4 cm long incision just above the kneecap.
One advantage is that the graft can be harvested either with or without a bone block from the kneecap. The graft, which is currently mostly used in revision cases (=second operations), has also been increasingly used as the graft of first choice in recent years.
There are usually no significant problems with the removal, unless the entire thickness of the tendon has to be removed, in which case rehabilitation is slower.
As with the patellar tendon, the disadvantage can be a loss of strength when extending the knee.
Allograft (donor tendon from a cadaveric donation): Thanks to newer methods of processing cadaveric tendons, there are hardly any disadvantages nowadays compared to autologous tendons. Due to a slightly higher rerupture rate (=new rupture of the transplant), this choice of transplant is reserved for revision surgery (=second operation) in order to avoid further weakening a joint through multiple tendon removal.
How is a cruciate ligament rupture operated on?
Nowadays, an individualized treatment approach is in keeping with the times. For me, it is no longer enough to use the same cruciate ligament transplant for every patient. Different bone sizes, leg axes, concomitant injuries or favored sports (jumping or sprinting) all play a role in the individual treatment algorithm.
In many cases, the anterior cruciate ligament does not tear singularly. Concomitant injuries such as meniscus tears, capsules or ligament injuries are common. Therefore, the timing of the operation should be considered, as well as any additional interventions to increase the stability of the joint.
To the arthoroscopic For arthroscopic cruciate ligament arthroplasty I use either the semitendinosus marriage (hamstring marriage) with the bone-sparing “all-in-side technique”, or a part of the quadriceps tendon. Both can be removed in a minimally invasive procedure.
The patient is placed in the supine position on the operating table and a tourniquet cuff is applied to the thigh of the leg to be operated on in order to temporarily interrupt the blood flow to the leg if necessary (this can be used for 2 hours without any consequences). In addition, the leg is placed in a pneumatically adjustable leg holder in order to be able to adjust the position of the legs comfortably during the operation.

During a diagnostic arthroscopy (= keyhole technique), the entire joint is inspected from the inside with a camera through skin incisions measuring just 2 x 0.5 cm. This means that injuries to the cartilage surface and meniscus tears can also be treated.
"All-in-side" technique using hamstring tendon
The “all in side” technique is one of the gentlest techniques in which the new cruciate ligament is pulled into short pre-drilled channels against 2 metal plates using the pulley technique and attached to the bone. Many conventional techniques require 2 tendons. With the gentle “all in side” technique, only one is needed (semitendinosus tendon). This means that the second of the hamstring tendons can be preserved.
I remove the semitendinosus tendon through a 2-3 cm long skin incision just above the popliteal fossa (= post-medial tendon removal). This allows me to spare a cutaneous nerve (infrapatellar ramus) which is damaged in up to 10% of cases by conventional harvesting. This can result in a loss of sensitivity on the inside of the lower leg.
The graft is prepared by specially looping the sutures with 2 adjustable suture loops (tightrope) to which 2 metal plates are attached. It is then moistened with an antibiotic solution to minimize the likelihood of bacterial colonization. The risk of infection can thus be reduced to almost zero.
Two bone channels are then created in the thigh and in the head of the tibia at the anatomical origin of the native cruciate ligament from the joint side in the same thickness as the harvested graft. After retracting the graft and flipping both metal plates on the outside of the bone, the graft can be retracted against the plates using the pulley technique .
ADVANTAGES OF THIS TECHNOLOGY
Anatomical positioning
Particularly strong primary fixation
Individually strong graft can be selected
Quadriceps tendon
For minimally invasive quadriceps tendon harvesting, an approx. 3-4 cm skin incision running vertically from the kneecap upwards is usually sufficient. Thanks to the special harvesting tool, a graft of varying thickness can be selected depending on body and bone size. Once part of the tendon has been removed, the resulting gap is closed. I also use a special suture loop for the quadriceps tendon, which is firmly sutured to the tendon. A small metal plate is attached to the adjustable suture loop (tightrope), against which the tendon can be firmly tightened using the pulley technique after it has been pulled into the bone. The quadriceps tendon graft is screwed into the tibial plateau with a bioabsorbable (= biodegradable polymer) interference screw.
Rehabilitation after cruciate ligament surgery
After arthoroscopic cruciate ligament surgery, patients can usually leave the hospital on the second day after the operation. Physiotherapeutic treatment takes place during the inpatient stay, but must be continued immediately afterwards in order to regain full freedom of movement as soon as possible.
A splint is not usually necessary. For accompanying meniscus sutures or cartilage surgery, immobilization with a motion orthosis and partial weight bearing with crutches is necessary during the first 6 weeks.
After a cruciate ligament injury, there is a higher risk of re-injury to the same knee, but also to the other knee. A cruciate ligament prevention program is therefore essential for further sporting activities.
Frequently asked questions about cruciate ligament surgery
Healing time after cruciate ligament surgery?
A cruciate ligament that has been operated on must first heal back into the bone before it can provide good long-term stability. This takes several months.
Milestones in rehabilitation:
- Full load within the first 2 weeks
- The patient is usually fit for work after 6-8 weeks
- Cycling is permitted after approx. 6-8 weeks
- Running only after 3 months
- It is possible to return to your usual sport after 6 months
- Ready for competition after 9-12 months at the earliest
How long do you need crutches after cruciate ligament surgery?
After a simple cruciate ligament replacement, you only need crutches for 2 weeks. If the meniscus has also been sutured, you usually have to use crutches for 6 weeks.
How soon after a cruciate ligament rupture does surgery need to be performed?
The operation should be performed eitherin the first 10 days or after the primary irritationhas subsided(approx. 6 weeks). If surgery is performed during the irritation phase, the likelihood of severe scarring of the entire joint (=arthrofibrosis) increases.
Does a cruciate ligament rupture always require surgery?
If the joint is unstable after a cruciate ligament rupture , surgery should be performed. If you are young and active in sports, surgery should be favored in order to avoid permanent damage. If the requirements are low, the patient is older and has little sporting ambition, and there is no tangible instability, conservative treatment can be chosen without any problems.
Can a cruciate ligament rupture heal without surgery?
The function of the cruciate ligament can sometimes be well compensated for by a strong muscle sheath. As the cruciate ligament lies in the middle of the joint and the joint is filled with synovial fluid, no haematoma can form, which is so important for healing. In individual cases, scarring can occur with the posterior cruciate ligament. However, functional healing of the anterior cruciate ligament after a complete tear is very unlikely.
How long in hospital after cruciate ligament surgery?
You should expect to stay in hospital for 1-2 days after a cruciate ligament reconstruction.