Shoulder dislocation
Shoulder dislocation
Acute care & follow-up treatment
ÜBERSICHT
A shoulder luxation (dislocation) usually occurs after a violent impact with excessive external rotation and spreading of the arm. The dislocation usually takes place forwards and downwards so that the labrum (a ring of connective tissue that surrounds and enlarges the socket) is separated from the socket (= Bankart lesion). Once the labrum has been torn off, it no longer heals in its original position on its own.
After repeated dislocations, the labrum degenerates completely until it is completely used up. Humeral head compression fractures (=HillSachse dent) are dents in the humeral head that occur when the humeral head strikes the bony glenoid cavity and leaves a dent in the softer bone there.
With frequent dislocations, not only can the labrum tear at the anterior and lower edge, a bony edge of the glenoid cavity can also break away, causing the glenoid cavity to become smaller again.
Consequences of injury after a shoulder dislocation:
- Bony defect of the joint socket (bony bench type)
- Torn labrum (Bankart lesion)
- Hill Sachs dent (dent of the humeral head)
- Avulsion fractures of the coracoid process (coracoid fracture)
- Tendon rupture of the subscapularis tendon (part of the anterior rotator cuff)
- Avulsion fractures of the tendon insertions ( tuberculum majus fracture)
The more concomitant injuries there are, the more likely a new injury is. All it takes is one small movement in everyday life and the shoulder pops out of its socket again. Every new dislocation can result in a new injury.
Diagnosis after a shoulder dislocation
During the clinical examination in my practice, I can determine whether there is instability with a few tests. After such an injury, it is also necessary to determine whether there is instability in only one direction or in several directions (unidirectional vs. multidirectional instability).
X-rays are essential after a fresh trauma in order to determine the position of the humeral head in relation to the glenoid cavity (joint concavity) and to detect any accompanying bony injuries.
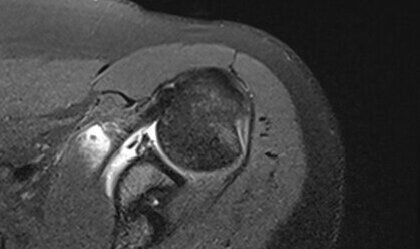
Magnetic resonance imaging (MRI ) should always be performed in order to detect the labral tear (Bankart lesion) that almost always occurs and to identify concomitant injuries. Tears of the rotator cuff are frequently found in older patients in particular and can usually be visualized very well with an MRI.
Shoulder dislocation therapy
The aim is a pain-free, weight-bearing shoulder with free mobility and minimal risk of a new dislocation. The probability of a new dislocation is around 90% in patients under 30 years of age, but decreases with increasing age. Physiotherapy is therefore usually the method of choice for older patients with lower demands on the shoulder.
The treatment plan is individualized depending on the age of the patient, the accompanying injuries and the requirements of the injured shoulder.
The most common procedure is labral refixation, in which the injured labrum is reattached to the joint socket and the joint capsule is slightly tightened as part of a shoulder arthroscopy (joint endoscopy). This is a relatively minor procedure that is sufficient in many cases.
However, a precise examination and measurement of the anatomy is required before surgery. If you already have a bony avulsion injury of the glenoid cavity, a dent in the humeral head (Hill Sachs dent), or both, simply attaching the labrum may no longer be sufficient.
